HIPAA Compliance in 2025: What Every Healthcare Provider Must Know

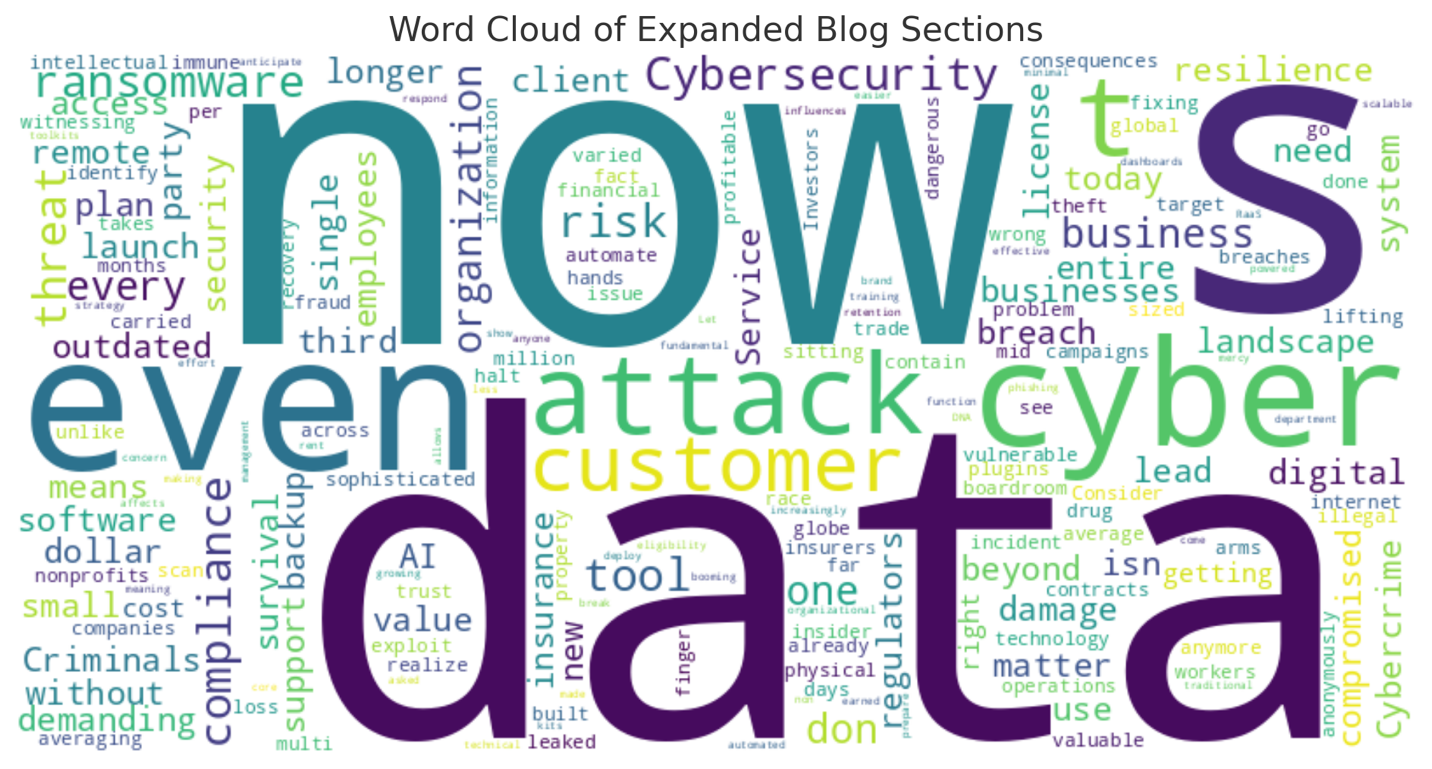
The Health Insurance Portability and Accountability Act (HIPAA) has always been a cornerstone of patient privacy and healthcare data protection. But in 2025, compliance is no longer just about having the right paperwork—it’s about managing cybersecurity, operational risk, and regulatory scrutiny in real time.
As ransomware attacks on hospitals rise and telehealth becomes more prevalent, healthcare providers—from private practices to large medical systems—must evolve their compliance strategies or risk severe penalties. With potential fines ranging from $137 to $50,000 per violation, and breaches now averaging $10.93 million in total damages, HIPAA is no longer a checklist—it's a critical business strategy.
Whether you're a physician group, clinic, health tech startup, or behavioral health provider, this guide breaks down what you need to know about HIPAA compliance in 2025 and how to protect your patients, your practice, and your bottom line.
2025 Trends Driving HIPAA Compliance Changes
Staying compliant with HIPAA isn’t just about checking boxes anymore—it’s about understanding how today’s risks and technologies are rapidly evolving. In 2025, healthcare providers are facing new pressures from cyber threats, expanded federal enforcement, and the digital transformation of patient care. Below are the top trends every organization must factor into their HIPAA strategy this year:
1. Ransomware & Cyber Attacks Are on the Rise
Healthcare remains the #1 most targeted industry for cyberattacks in 2025. Ransomware groups are becoming more sophisticated, with some using AI to bypass traditional defenses and exploit outdated systems.
- Healthcare breaches have risen over 130% since 2020, with attacks lasting an average of 15 days and costing $10M+ per incident.
- The FBI and HHS have issued joint warnings about “data double extortion” schemes, where attackers not only encrypt records but threaten to publicly release patient data unless paid.
- Small and mid-sized providers are increasingly at risk due to limited IT budgets and aging infrastructure.
Implication: Without a robust cybersecurity posture—including endpoint protection, MFA, and encrypted backups—providers could face irreparable data loss, HIPAA fines, and patient lawsuits.
2. Telehealth Expansion Requires New Safeguards
The post-pandemic boom in telehealth has shifted how providers interact with patients. While virtual visits offer convenience, they also expand your HIPAA attack surface.
- Video platforms, remote EHR access, third-party health apps, and mobile device usage all increase potential exposure.
- In 2024, HHS allowed certain COVID-era enforcement flexibilities to lapse—meaning 2025 is the first full year of restored HIPAA enforcement for telehealth.
- The use of personal devices by providers and staff for patient communication must now be covered by strict BYOD policies and security protocols.
Implication: If your telehealth system isn’t encrypted, monitored, and covered by business associate agreements (BAAs), you may be out of compliance.
3. Increased HHS Audits & Enforcement
The HHS Office for Civil Rights (OCR) has dramatically increased the number of random and complaint-based audits in 2025. They are particularly targeting:
- Practices with known breaches or poor audit history
- Providers using new tech platforms (like AI or cloud-based EHRs)
- Entities with previous failure to conduct a proper Security Risk Assessment (SRA)
OCR now expects providers to produce full documentation of their compliance activities within 10 business days of notice.
In 2025, more audits are initiated from patient complaints—including perceived mishandling of data, delayed records access, or unauthorized disclosures.
Implication: If you can't produce your SRA, training logs, or up-to-date policies, your practice may be subject to significant penalties—even if no breach has occurred.
4. Growth of Third-Party Vendors & BAAs
Healthcare is becoming more interconnected, with practices outsourcing everything from billing to cloud hosting to AI triage systems.
- This creates long chains of data handlers, all of which must be covered by Business Associate Agreements (BAAs).
- Many providers still fail to track or update BAAs, leaving them vulnerable if a vendor mishandles data.
Example: If your EHR platform or billing company is breached and you don’t have a signed, HIPAA-compliant BAA, your practice—not the vendor—will bear legal responsibility.
Implication: You must manage and review BAAs annually and ensure that subcontractors of business associates are also compliant.
5. Legal & Insurance Industry Pressures Are Mounting
In 2025, HIPAA compliance is increasingly linked to malpractice risk, insurance underwriting, and even M&A activity.
- Cyber liability insurers now require HIPAA SRAs and technical safeguards before issuing policies.
- Investors and acquirers are demanding HIPAA audits as part of due diligence for practice acquisitions.
- State attorney generals in New York, California, and Illinois are stepping up enforcement at the state level, often exceeding federal standards.
Implication: HIPAA non-compliance may not just result in regulatory fines—it could cost you insurance coverage, business growth opportunities, or lead to personal legal exposure.
HIPAA Compliance Checklist for 2025
Here is an updated HIPAA compliance checklist every provider should review this year:
- Perform a Security Risk Assessment (SRA)
- Maintain Updated Policies & Procedures
- Train Employees and Contractors Regularly
- Review and Enforce Business Associate Agreements (BAAs)
- Implement Technical Safeguards
- Prepare an Incident Response and Breach Notification Plan
- Use a Compliance Management System (CMS)
Each of these steps is mandatory under HIPAA—and failing even one can trigger enforcement.
Common HIPAA Mistakes to Avoid in 2025
Even well-meaning practices make mistakes that can result in costly penalties or lawsuits. Here are the top red flags ATG encounters:
| Mistake | First Name |
|---|---|
| No annual SRA | Required under HIPAA; first thing HHS asks for during audit |
| Outdated Policies | Makes your defense invalid in the event of breach |
| Missing BAA with IT vendors | Results in full liability for third-party violations |
| Untrained staff | Leads to phishing attacks and improper data sharing |
| No breach response plan | Slows containment and increases damage |
| Poor email security | Unencrypted PHI transmission is a common violation |
Penalties for HIPAA Non-Compliance
| Tier | Penalty per Violation | Max Annual Penalty |
|---|---|---|
| Tier 1 | $137 – $1,379 | $27,500 |
| Tier 2 | $1,380 – $13,785 | $110,000 |
| Tier 3 | $13,786 – $50,000 | $1.1 million |
| Tier 4 | Willful Neglect | $50,000+ |
In addition to federal penalties, you may also face:
- Patient lawsuits
- State regulatory action
- Malpractice exposure
- Public relations damage
Case Study: How ATG Advisors Helped a 25-Employee Medical Practice
The Situation:
A dermatology practice experienced a breach due to an unsecured remote desktop connection managed by their outsourced IT vendor.
What We Found:
- No current SRA
- No BAA with vendor
- Outdated training program
- Weak password protocols
What We Did:
- Emergency mitigation & HHS coordination
- Full HIPAA compliance rebuild
- Vendor review & new IT infrastructure
- Cyber liability insurance coordination
Outcome:
The practice passed follow-up audits with no fine and is now a model of compliance in its specialty.
How ATG Advisors Can Help
We specialize in HIPAA compliance solutions for modern practices, including:
- 🔍 Annual HIPAA Risk Assessments
- 📄 Policy & Procedure Templates
- 🤝 BAA Management & Vendor Vetting
- 💻 IT Security Audits & Infrastructure Reviews
- 🎓 Employee Cybersecurity Training
Ready for Your HIPAA Checkup?
Let ATG Advisors help you audit, strengthen, and secure your entire compliance operation.
📅
Schedule a free consultation
📧 Email: info@atgadvisors.com
📞 Phone: 704-957-5194
Related Resources
- “HIPAA for Small Practices: The 2025 Guide”
- “The Cost of a Breach: Lessons from Real Healthcare Incidents”
- “Cybersecurity in Healthcare: What You’re Legally Required to Do”