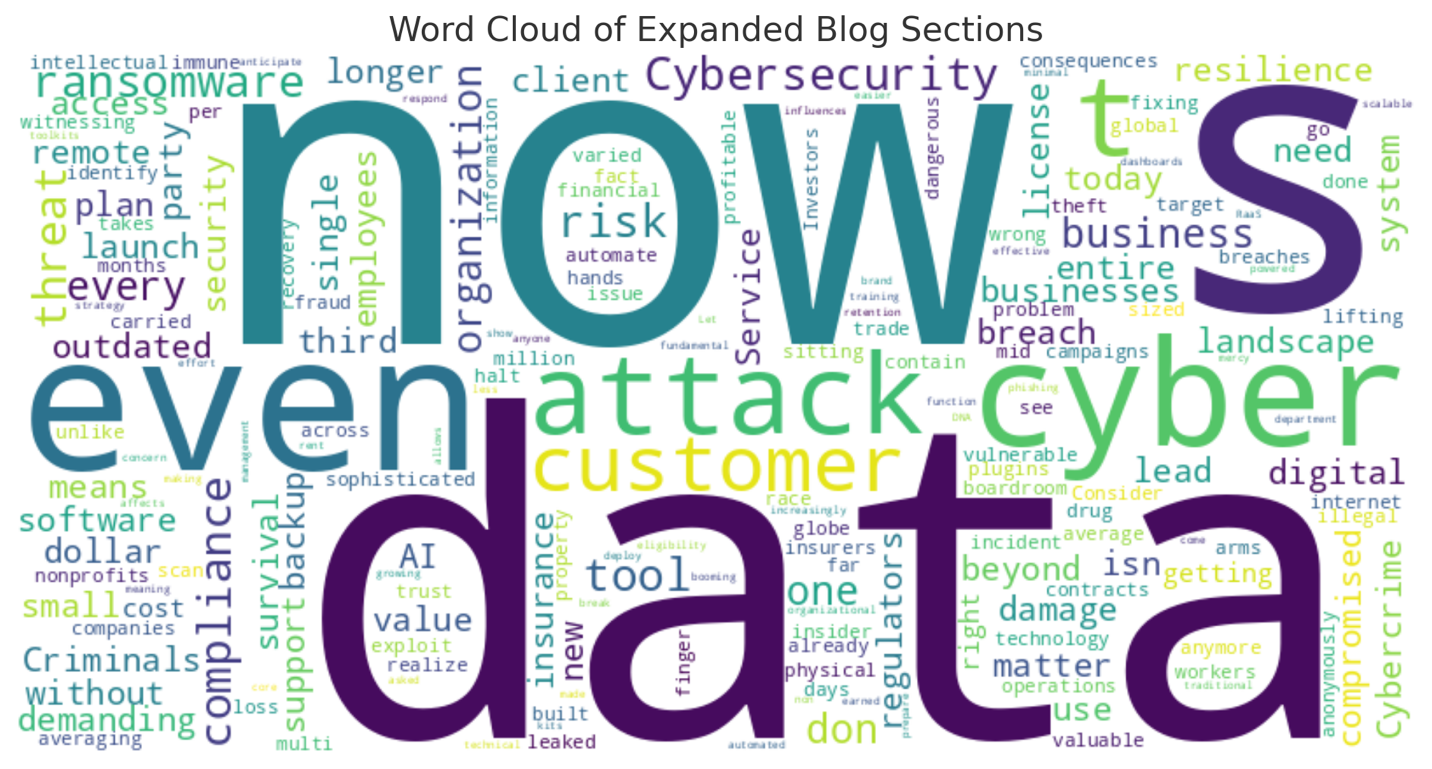
Compliance in Crisis: Navigating Defunding & Government Restructuring in 2025 – A Healthcare Perspective
A New Era of Financial Uncertainty
In 2025, healthcare providers across the United States are facing an unprecedented challenge: widespread defunding of critical government programs. From Medicaid reimbursement adjustments to the restructuring of the Department of Health and Human Services (HHS), the healthcare landscape has entered a volatile phase. Compliance officers, CFOs, and operations executives are scrambling to keep pace with shifting policies, dwindling support, and rising demand for patient care.
This blog explores how healthcare organizations can maintain compliance, optimize funding strategies, and build resilience in a time of systemic change. We'll walk through the current risks, real-world examples, and how ATG Advisors partners with hospitals, clinics, and public health systems to adapt with confidence.

The Funding Cliff: What’s Actually Being Cut in 2025
The 2025 federal budget slashed over $11 billion in public health funding, including reductions in the CDC’s vaccination initiatives and HRSA grants for rural health outreach. Simultaneously, the HHS realignment merged several regulatory units, creating confusion around reporting structures and compliance enforcement.
Programs affected include:
- Medicaid DSH payments
- Rural clinic stabilization grants
- FEMA hospital disaster reimbursements
Case Example:
A mid-sized hospital in the Midwest saw a 40% delay in FEMA reimbursements for tornado response services rendered in 2023. With payroll due and suppliers pressing, the CFO was forced to secure bridge loans, costing over $250,000 in interest fees over eight months. This delay became not just a budget issue but a reputational one, as the community noticed service cutbacks while demand surged.
Top Compliance Risks for Healthcare Providers
The defunding and agency restructuring underway in 2025 have triggered a domino effect of compliance and operational threats. Here are the most significant:
- Regulatory Confusion
With HHS reorganizing departments, guidance on reporting deadlines, HIPAA updates, and grant eligibility is fragmented. Healthcare executives are being asked to interpret changing policies without clear technical assistance. - Audit Vulnerability
Healthcare systems with outdated policy manuals or insufficient audit trails are failing OIG and state-level reviews. Noncompliance can lead to clawbacks, fines, and public audit failures that damage reputation. - Delayed Reimbursements
CMS and FEMA payment cycles are stretched. Many hospitals are now waiting 6 to 9 months for funds, forcing CFOs to burn reserves or secure short-term loans at high interest. - Untracked Grants
Smaller providers lack the systems to track grant compliance obligations under HRSA, SAMHSA, or NIH awards. This opens the door to funding ineligibility or audit exposure. - Workforce Instability
Clinical and administrative staff are being stretched thin by compliance ambiguity, reduced funding, and shifting roles. Burnout, turnover, and lack of training are leading to critical process gaps. - Technology Misalignment
Many healthcare organizations are still relying on outdated EHR and compliance systems that can’t meet modern interoperability or audit trail demands. This lack of integration makes it difficult to respond to audits, track grant funds, or meet real-time reporting requirements. - Overlapping Oversight
Providers face scrutiny from federal, state, and private payors, often with conflicting compliance rules. This duplicity in oversight creates inefficiencies and increases the chance of error.
Case Study:
A California-based community health center failed a state audit due to noncompliance with updated Title X reporting rules. The organization was fined $112,000 and had its reproductive health program suspended for three months, impacting care access for over 1,200 patients.
Strategic Solutions from ATG Advisors
At ATG Advisors, we don’t just help clients survive compliance shifts—we help them leverage this moment for strategic growth and operational modernization.
1. Compliance Readiness Audit
- Comprehensive review of internal policies, financial documentation, and federal program obligations.
- Implementation of updated compliance calendars and workflow automations tailored to federal and state deadlines.
2. Adjunct CFO Services
- Forecast cash flow with adjusted funding timelines and grant delivery schedules.
- Realign program budgets, payroll, and procurement with new revenue realities.
- Evaluate debt vs. reserve financing strategies to stay solvent without overleveraging.
3. Grant Optimization Support
- Realignment of service delivery models to match new allowable cost structures.
- Identification of private grants, foundation support, and state-level opportunities to close federal gaps.
- Real-time tracking of expenditures and grant milestones using cloud-based dashboards.
4. Continuity & Risk Mitigation Planning
- Creation of multi-scenario contingency plans for loss of key grants or payment delays.
- Workforce modeling to scale staffing with compliance and clinical delivery needs.
- Public relations and board briefings to ensure external trust during service interruptions.
5. Digital Infrastructure Modernization
- Conduct a technology audit to identify gaps in compliance tracking, documentation, and EHR integrations.
- Deploy or recommend cloud-based tools that meet HIPAA and audit-readiness needs.
6. Board & Stakeholder Education
- Deliver executive briefings and compliance updates for board members and senior leaders.
- Build awareness of funding risks and advocate for internal policy modernization.
Real-World Impact:
One of our client organizations—a safety-net hospital in the Southeast—used our continuity plan to avoid disruption when their HRSA grant was cut by 30%. By reallocating funds, fast-tracking a new state partnership, and launching a community donation campaign, the hospital maintained operations with no reduction in patient services.
Conclusion: Future-Ready Healthcare Begins with Action Today
The healthcare sector can no longer afford to operate on assumptions that funding or oversight will remain consistent. Leadership teams must move away from reactive management to data-driven, forecast-ready governance. ATG Advisors has the tools and insight to guide that transformation.
Our partners include health systems navigating complex grant portfolios, FQHCs adjusting to new HHS structures, and clinics balancing care delivery with compliance overload. Whether your challenge is financial, operational, or regulatory, ATG is equipped to respond with precision and urgency.
The only way to face regulatory chaos and funding shortfalls is with discipline, foresight, and support. ATG Advisors has guided hundreds of organizations through fiscal crises, audit stress, and operational gridlock—and we’re prepared to do it again.
If your health system, FQHC, or clinic is concerned about staying compliant, financially stable, or mission-driven amid federal changes, now is the time to act. Schedule your compliance audit or financial strategy session today—and turn uncertainty into momentum.
Contact ATG Advisors
Let’s build your compliance shield and operational game plan—before the next disruption.
Because when compliance breaks down, care delivery isn’t far behind.